When discussing immune cell therapies, it is almost impossible not to mention cytokine release syndrome (CRS), one of the most well-known adverse effects within immunotherapies. CRS involves the uncontrolled release of pro-inflammatory cytokines such as TNF-α and Interleukin (IL)-1, IL-2, and IL-6, among others.
When discharged together and in excess, these cytokines initiate the rapid onset of fever and other general symptoms that may easily transform into cardiorespiratory organ dysfunction and failures.
For the cell therapies that are approved at present, such as chimeric antigen receptor (CAR) T cell therapy, the onset of CRS is very common, with more than two-thirds of patients experiencing symptoms related to CRS and 23% of patients experiencing at least Grade 3 CRS symptoms.
As a result, practitioners are continuously pursuing novel ways to control CRS response while researchers are seeking to develop safer cell therapies.
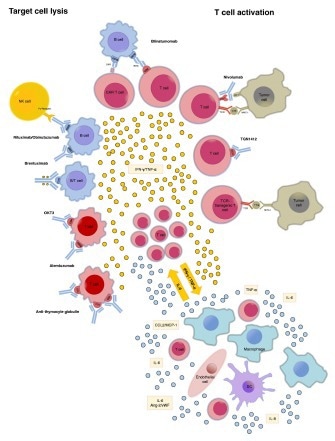
Image Credit: ACROBiosystems
Balancing risk and benefit
As with any type of pharmaceutical treatment regimen, balancing both therapeutic efficacy and adverse effects is of the utmost priority.
Regarding cancer treatment, particularly relapsed or refractory cancers, there are specific calculated risks that allow certain cell therapies to be approved.
However, this is accompanied by numerous considerable limitations, including drug concentration (quantity of infused CAR cells) and drug exposure time (dosing regimen).
As a result of these limitations, cell therapy treatment strategies are heavily reliant on monitoring CRS onset and severity, both common occurrences that can lead to the abandonment of CAR cell infusion.
CAR-NK (natural killer) cell therapies
CAR-NK is a novel exploratory region of cell therapies. Usually, natural killer (NK) cells are difficult to enrich, representing only 10% of lymphocytes, which further decreases the efficacy of leukapheresis and strains the manufacturing capacity.
However, a new cell line, NK92, has been developed. It is obtained from non-Hodgkin’s lymphoma and acts as an NK-like cell with pre-activated abilities.
With the advent of the NK92 cell line, CAR-NK has started to enter clinical phases with the general assumption that this type of CAR immune cell does not induce CRS.
It must be noted, however, that CAR-NK does not eradicate the secretion of cytokines, but instead has a different cytokine secretion profile that does not involve the usual inducers for CRS (e.g., IL-6). This means the risk of CRS is lessened but not excluded, but with an equal level of severity, giving a comparable limitation to alternative cell therapies.
In experimental CAR NK92 clinical trials, CRS incidence has been reported. In a phase II clinical trial, one patient experienced a sequence of unexpected symptoms, developing into hypotensive shock, myalgia, high fever, and abnormal blood.
From the additional analysis of serum cytokine levels, it was revealed that IFN-γ and TNF-α were raised with no significant difference in IL-6. Although IL-6 is a key driver in the inflammatory symptoms correlated with CRS, the elevated concentration of cytokines may also cause a CRS-like sequence of adverse side effects.
CRS is still not exhaustively understood. This is partly a result of the intricate interconnective cytokine signaling pathways and the specific clinical effects caused by secreted cytokines.
Clinical guidelines of CRS
With the advancement of novel, alternative immune cell therapies with a distinct cytokine secretion profile, another important area of improvement is present CRS management strategies. This involves CRS diagnostics, grading, and proposed strategies for treatment.
The current algorithm has recently been updated for its implementation in CAR-T clinical trials, focused on clinical symptoms such as fever and organ dysfunction, as well as monitoring at least two cytokine profiles.
However, with the introduction of CAR-NK, the selected cytokine profiles most likely to cause CRS are still uncertain.
Another major concern is the algorithm for standardized protocol treatment for severe CRS. Tocilizumab is an FDA-approved antibody that binds to the IL-6 receptor and has been demonstrated to be extremely successful in ameliorating CRS symptoms.
However, the case study outlined in this article does not display a clear elevation of IL-6, which minimizes the efficacy of a first-line CRS treatment drug.
As a result, the advancement of early detection and symptomatic management of CRS unique to NK cells may be another area of focus to help inhibit major CRS toxicities in next-generation immune cell therapies.
Driving clinical research for cytokine diagnostic biomarkers
With the increase in CAR-NK and the research into other CAR-NK cell therapies, understanding the cytokine signaling pathway is essential: not only for learning the biological effects but also in the clinical space for diagnostics and treatment strategies.
Identification of immune-cell specific or a set of cytokines can facilitate the diagnosis of CRS and enable monitoring with newer, real-time diagnostic technologies. This means testing a wider variety of cytokines than the typical CAR-T CRS panel that includes IL-6.
ACROBiosystems offers a broad range of various reagents for the detection of cytokines to aid all applications, from research and development to clinical research.
About ACROBiosystems
ACROBiosystems is a leading manufacturer of recombinant proteins and other critical reagents to support the development of target therapeutics. The company employs an application-oriented development strategy, with a particular focus on product design, quality control, and solution-based support. Our products and services enable anyone in the field of drug development to have a more intuitive and streamlined process.
To respond to the coronavirus pandemic, ACROBiosystems has developed SARS-CoV-2 antigens specifically designed and optimized for serological test kits, including Spike-derived antigen S1, RBD, and Nucleocapsid protein. Proteins have been supplied to diagnostic companies in large quantities.
Sponsored Content Policy: News-Medical.net publishes articles and related content that may be derived from sources where we have existing commercial relationships, provided such content adds value to the core editorial ethos of News-Medical.Net which is to educate and inform site visitors interested in medical research, science, medical devices and treatments.